Toward health equity: trauma and violence informed care (TVIC)
Learn more about what it means to add 'violence' to being trauma informed
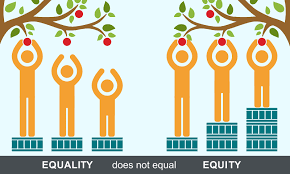
The 21st century understanding of family violence is moving toward being trauma and violence informed.[See the Vega Project] At the heart of it, TVIC means treating people like whole human beings deserving of respect, support and dignity, no matter their circumstances – regardless of their gender, age, race, ability, sexual orientation or economic situation. The measure of TVIC lies in the policies and practices that impact on clients. Professionals and organizations can assess TVIC readiness by looking at the ways in which the day-to-day business of the agency is carried out.
Adding the “v” to trauma-informed
From: Equip Health Care online modules
- Trauma-informed care seeks to create safe environments for clients based on understanding the effects of trauma and links to health and behaviour
- Trauma and violence informed care expands this concept to account for intersecting effects of systemic and interpersonal violence
- Professionals who are aware of trauma and violence in the populations they serve can help clients to feel safe in the care environment
- Professionals who practice TVIC report higher morale and job satisfaction and increased collaboration with clients
Four ways to work in a trauma and violence informed way
Build awareness and understanding of:
- The high prevalence of trauma and violence
- The significance of historical (collective and individual) and ongoing violence (interpersonal and systemic)
- How the impact of trauma can be central to one’s development
- The wide range of adaptations people make to cope and survive
- The relationship of trauma and violence with substance use, physical health and mental health concerns
Emphasize safety and trust:
- Create welcoming environments and intake procedures
- Adapt the physical space for comfortable and private interactions
- Communication clear and accurate expectations about services
- Ensure informed consent and confidentiality
- Help create crisis and safety plans
- Understand the history and context of individuals and groups
- Think of these strategies as “universal precautions” to ensure all clients are not re-traumatized or harmed.
Adapt your language:
- Use non-stigmatizing language everywhere – from signage, to intake forms and how client’s situations are discussed
- Use the names and pronouns transgender youth choose for themselves
Consider trauma a risk factor:
- For physical health problems
- For smoking, heavy drinking, drug use and high risk sexual behaviours to cope with emotional and physical pain
- Experiences of sexual violence, racism and discrimination can change neurological patterns and genetic structures that affect mental and physical health
Watch Jim Hopper talk about being trauma-informed in the context of investigations: